 The ultimate guide to taking control of your health and beauty during menopause
The ultimate guide to taking control of your health and beauty during menopause
testimonials
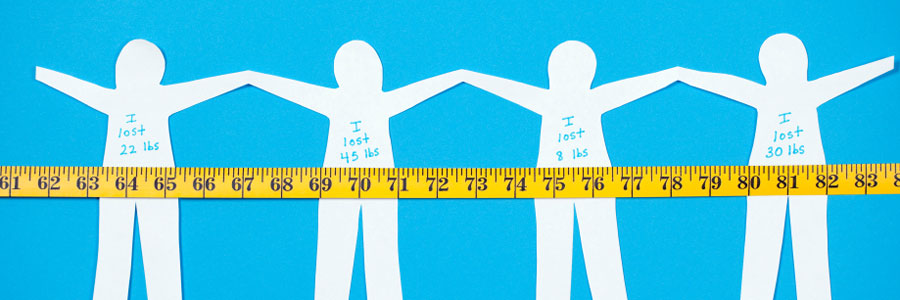
 Age: 53 I am here to tell you the incredible truth. Twelve weeks after starting The Menopause Makeover... I lost 22 pounds!
That is just unbelievable. The boost in energy I feel is great! The fatigue is gone. I am energized. My emotions are stable, even upbeat and giddy sometimes!
It's been a decade of struggle. I've been fighting depression, and hot flashes for many years.
Age: 53 I am here to tell you the incredible truth. Twelve weeks after starting The Menopause Makeover... I lost 22 pounds!
That is just unbelievable. The boost in energy I feel is great! The fatigue is gone. I am energized. My emotions are stable, even upbeat and giddy sometimes!
It's been a decade of struggle. I've been fighting depression, and hot flashes for many years.
 My self-image was sharply deflated, and as a single working mom at 53, I had little time, and no energy to devote to myself. I have never had any success with weight loss.
Staness, the amazing makeover queen, has given me the tools to lose the weight.
The Menopause Makeover Food Pyramid has been a formula that suits me perfectly. I don't get sluggish and grumpy.
Thank you Staness for creating a sensible and balanced way to LIVE. Not only through menopause, but forever!
I feel wonderful. My life looks and feels better than ever!
My self-image was sharply deflated, and as a single working mom at 53, I had little time, and no energy to devote to myself. I have never had any success with weight loss.
Staness, the amazing makeover queen, has given me the tools to lose the weight.
The Menopause Makeover Food Pyramid has been a formula that suits me perfectly. I don't get sluggish and grumpy.
Thank you Staness for creating a sensible and balanced way to LIVE. Not only through menopause, but forever!
I feel wonderful. My life looks and feels better than ever!
Share YOUR story! Email Staness@MenopauseMakeover.com
Turkey Chili
 This is my all-time favorite chili recipe. The good news is that chili is not only comfort food, but it can be healthy, too!
This is my all-time favorite chili recipe. The good news is that chili is not only comfort food, but it can be healthy, too!
Chili contains lots of protein. This recipe is made with turkey, so it is a leaner alternative to ground beef. Chili can help you lose weight. The “capsaicin,” a colorless compound found in the chilies used to season this dish, can increase your metabolic rate by increasing your body heat production. Chili is also high in iron thanks to the turkey and beans and has vitamin C thanks to the tomatoes, peppers and chilies. Plus, it’s a great source of fiber that helps keep you feeling full for a long time after eating. Enjoy the healthy benefits of chili!
8-10 servings prep time = 30 minutes Ingredients 2 medium onions, chopped (1 cup) 1 tablespoon vegetable oil 2 tablespoons chopped fresh garlic 1 medium red bell pepper, chopped (1 cup) 1 medium green bell pepper, chopped (1 cup) 2 pounds ground turkey 2 tablespoons ground cumin 1 tablespoon dried oregano leaves 1 tablespoon chili powder 1 can (4 ounces) chopped green chilies, drained 2 jalapeño chilies, seeded and chopped 28-oz. can of whole Roma (plum) tomatoes 3 cups water for thick meaty chili, or 4 cups for “soupier” chili 2 cans (15 ounces) black beans, drained 1 can (15 to 16 ounces) kidney beans, drained Salt and pepper to taste Sweet onions, sliced Low-fat sour cream Directions -Cook the onions in vegetable oil in a large saucepan over medium heat for about 10 minutes or until the onions are tender. -Add garlic and the green and red bell peppers, cook 2 to 3 minutes. -Add turkey and cook 3 to 4 minutes or until the turkey is no longer pink. -Add cumin, oregano, chili powder, green chilies, jalapeño chilies, tomatoes and water. Reduce heat to low. -Cover and simmer about 30 minutes. -Add beans; simmer 15 to 20 minutes longer. I simmer for a total of 2 hours for a rich flavor. -To serve, add sliced sweet onions to the top and a dab of low-fat sour cream. If you want to make this recipe spicy, add one whole red habeñero or one whole serrano chili (deveined, deseeded and chopped). Or if you like a Tex-Mex flavor, add an envelope of taco seasoning as you simmer this recipe. Calories 175 Protein 15 grams Carbs 13 grams Fat 6 grams Fiber 5 grams By Staness Jonekos, The Menopause MakeoverPerimenopausal Depression
 Are you suffering from hot flashes, night sweats, or cranky moods? Feeling hopeless, apprehensive, or deep sadness for prolonged periods? If so, you may be suffering from perimenopausal depression.
Depression is more common among women than men. Biological, life cycle, hormonal, and psychosocial factors that women experience may be linked to women's higher depression rate. Researchers have shown that hormones directly affect the brain chemistry that controls emotions and mood.
Perimenopausal symptoms may be the cause of depression, and for some, it may ever be clinical depression.
According to the North American Menopause Society:
Are you suffering from hot flashes, night sweats, or cranky moods? Feeling hopeless, apprehensive, or deep sadness for prolonged periods? If so, you may be suffering from perimenopausal depression.
Depression is more common among women than men. Biological, life cycle, hormonal, and psychosocial factors that women experience may be linked to women's higher depression rate. Researchers have shown that hormones directly affect the brain chemistry that controls emotions and mood.
Perimenopausal symptoms may be the cause of depression, and for some, it may ever be clinical depression.
According to the North American Menopause Society:
Women who had severe PMS in their younger years may experience more severe mood swings during perimenopause. There are many factors that can cause an increased risk for depression from your genes, to having a prior history to taking certain medications. Certain endocrine disorders, such as hypothyroidism, or other illnesses, such as chronic fatigue syndrome, are also associated with depression. Signs and symptoms include:A depressed mood --This is a normal, brief period of feeling blue or sad that is commonly experienced and rarely requires treatment.
Depression as a symptom – This type of depression may be due to a wide variety of medical or psychological problems, or to intense reactions to life events (such as divorce, losing a job, death of a loved one). It is usually short-term and most often does not require treatment, although it can progress to clinical depression.
Clinical depression -- This is a pathologic disorder believed to result from a chemical imbalance in the brain. A clinical (major) depression requires treatment.
- Persistent sad, anxious, or "empty" feelings
- Feelings of hopelessness or pessimism
- Feelings of guilt, worthlessness, or helplessness
- Irritability, restlessness
- Loss of interest in activities or hobbies once pleasurable, including sex
- Fatigue and decreased energy
- Difficulty concentrating, remembering details, and making decisions
- Insomnia, early-morning wakefulness, or excessive sleeping
- Overeating, or appetite loss
- Thoughts of suicide, suicide attempts
- Aches or pains, headaches, cramps, or digestive problems that do not ease even with treatment.
According to the Study of Women’s Health Across the Nation (SWAN): The risk of major depression is greater for women during and immediately after the menopausal transition than when they are pre-menopausal. If you suffer from depression whether mild, moderate or clinical, get support and visit your health care provider to discuss your options. By Staness Jonekos Co-Author, “The Menopause Makeover”If you are still feeling very stuck and sad, talk to your clinician so you can get a referral to a good psychotherapist. If you need medication, in the broader context of menopausal symptoms, there is some evidence that hormone therapy can augment treatment and help people who are on anti-depressants feel even better. That is a decision for you and your clinician.
Menopausal Weight Gain: How To Get Your Body Back
 It is estimated that the average weight gain during the menopause transition is about 10 to 15 pounds. Well, I must not be average, because I gained almost 30 pounds in less than a year when I slammed into menopause! Frustrated that I could not find a solution, I sacrificed myself as a human guinea pig and figured out how to lose it all in just 12 weeks.
To be successful, weight loss during menopause demands a new strategy. It takes more than cutting calories to lose weight during this life transition! I was surprised to discover, according to new research, that for many women menopausal weight gain is not entirely their fault.
The first culprit is aging. Both men and women lose muscle mass as they age, which can lower the body’s resting metabolism, therefore increasing the risk of weight gain and accumulating body fat around the waist.
Many women become less physically active in their 40s, 50s and 60s because life is busy; it’s a challenge to find time to schedule exercise. Less activity means less muscle mass, which means weight gain.
Now get ready for the double whammy: Aging plus hormone changes.
Studies claim that the perimenopause transition may contribute to increased fat in the abdomen, changing a woman’s shape from a pear to an apple with more of the fat disturbed around the waist. Here’s proof that weight loss is an uphill battle.
As we age and slide into menopause, it is suspected that declining estrogen levels may lower the rate of energy used during exercise. Weight loss habits and workout routines used in younger years often aren’t as effective as we age. It takes more work to lose weight. Not achieving your desired results within a certain time frame may increase frustration and decrease motivation.
Declining estrogen levels wreak hormonal havoc that can cause night sweats, and that is a formula for sleepless nights. Sleep deprivation produces increased levels of ghrelin – the hunger hormone – and decreased levels of leptin – the “stop eating” hormone. This can equal weight gain.
The list continues. Grab a glass of wine and settle in:
It is estimated that the average weight gain during the menopause transition is about 10 to 15 pounds. Well, I must not be average, because I gained almost 30 pounds in less than a year when I slammed into menopause! Frustrated that I could not find a solution, I sacrificed myself as a human guinea pig and figured out how to lose it all in just 12 weeks.
To be successful, weight loss during menopause demands a new strategy. It takes more than cutting calories to lose weight during this life transition! I was surprised to discover, according to new research, that for many women menopausal weight gain is not entirely their fault.
The first culprit is aging. Both men and women lose muscle mass as they age, which can lower the body’s resting metabolism, therefore increasing the risk of weight gain and accumulating body fat around the waist.
Many women become less physically active in their 40s, 50s and 60s because life is busy; it’s a challenge to find time to schedule exercise. Less activity means less muscle mass, which means weight gain.
Now get ready for the double whammy: Aging plus hormone changes.
Studies claim that the perimenopause transition may contribute to increased fat in the abdomen, changing a woman’s shape from a pear to an apple with more of the fat disturbed around the waist. Here’s proof that weight loss is an uphill battle.
As we age and slide into menopause, it is suspected that declining estrogen levels may lower the rate of energy used during exercise. Weight loss habits and workout routines used in younger years often aren’t as effective as we age. It takes more work to lose weight. Not achieving your desired results within a certain time frame may increase frustration and decrease motivation.
Declining estrogen levels wreak hormonal havoc that can cause night sweats, and that is a formula for sleepless nights. Sleep deprivation produces increased levels of ghrelin – the hunger hormone – and decreased levels of leptin – the “stop eating” hormone. This can equal weight gain.
The list continues. Grab a glass of wine and settle in:
- Loss of estrogen may make insulin less effective at lowering glucose, and more effective at storing fat.
- Suffering from menopausal symptoms can affect a woman’s emotional health…weight goes up, self-esteem goes down.
- Normal life and environmental changes, such as children leaving or coming back home, divorce, death, career changes, can be stressful.
- The stress hormone, cortisol, directly affects fat storage and weight gain in stressed individuals. Cortisol is associated with increased appetite, cravings for sugar, and weight gain.
- There's a link between estrogen and body fat storage. Post-menopausal women burn less fat than they did in their pre-menopausal years. Cells not only store more fat but are less willing to part with it.
- Medical conditions such as insulin resistance (when your body becomes resistant to the insulin it produces) or suffering from an underactive thyroid can pack on the pounds.
- Medications that can trigger appetite, slow metabolism, increase fluid retention, and cause muscle cramps decreasing desire to exercise are: antidepressants, antihistamines, beta-blockers, corticosteroids, insulin, statins and tamoxifin.
- Eat Protein: Women naturally have less muscle mass and testosterone than men, so lean proteins such as, chicken, turkey, fish, beans, soybeans and tofu, dairy protein/Greek yogurt, low fat cottage cheese, egg whites, are a woman’s best friend during menopause. Your body expends more energy (calories) to process proteins.
- Consume healthy fats: olive oil, flaxseeds, salmon, halibut, tuna, avocados, almonds, and walnuts.
- Manage blood sugar with low to medium glycemic index foods: beans, apples, oranges, cherries, plain yogurt, sweet potatoes, oatmeal.
- Fiber is your friend keeping you feeling full longer and regular.
- Limit alcohol to 2 or less glasses per day: That totals less than 10 fluid ounces of wine, 24 ounces of beer, or 3 ounces of 80-proof distilled spirits. More than two drinks per day may increase the risk of cancer and stroke.
- Don’t smoke.
- Watch salt intake to reduce fluid retention.
- Practice portion control. Using smaller plates can help.
- Keep a food diary and create a food plan. There are many great apps for your mobile that may help.
- Eat every 3-4 hours so you don’t get hungry. Three meals and two snacks per day (three if you wake up early).
- Exercise at least 30 minutes most days of the week to maintain a healthy weight; increase workout time if your goal is to lose weight.
- Make breakfast and lunch your largest meals.
- Nourish healthy emotions: are you happy, are you surrounded by healthy relationships, is your self esteem high?
Will Your Marriage Survive Menopause?
 Over 60 percent of divorces are initiated by women in their 40s, 50s or 60s — the menopause years — according to a recent survey conducted by AARP Magazine. Why are women running away from marriage?
Over 60 percent of divorces are initiated by women in their 40s, 50s or 60s — the menopause years — according to a recent survey conducted by AARP Magazine. Why are women running away from marriage?
Ankle Osteoarthritis and Stem Cell Therapy
 My future was changed forever when I sprained my ankle in a college ballet class. This injury was 40 years ago yet a third degree sprain like mine was treated the same way as today: P-R-I-C-E (protect from further injury, restrict activity, apply ice, apply compression, and elevate the injured area).
Little did I know that the ligaments I injured had started physiological changes that would compromise my joint stability. The healing response that was initiated in an attempt to repair the damage actually increased my risk for degenerative changes that eventually led to osteoarthritis. It is the most common type of arthritis caused by the degradation of a joint’s cartilage. There are up to two million acute ankle sprains each year in just the USA alone.
Fifteen years after the initial ankle sprain I had severe pain and was forced to seek out medical attention in an attempt to walk normally again. Being in my mid-thirties and hearing that my only option was an ankle fusion, limiting motion for the rest of my life, was devastating news. My new mission was to find an ankle expert that was a pioneer.
NOTE reference photo of my left ankle X-ray 40 years after the injury, bone on bone, compared to a healthy normal ankle on the right side.
After five appointments with orthopedic surgeons in the Los Angeles area, I discovered Dr. Richard Ferkel at the Southern California Orthopedic Institute (SCOI). He became my lifetime ankle hero. He specializes in arthroscopic and reconstructive surgery of the ankle, as well as cartilage restoration, but it was his work with the U.S. Olympic teams, the NFL and NBA that really impressed me. If professional athletes entrusted their careers and joints to him, so would I.
Dr. Ferkel did a procedure to clean up the bone spurs, called arthroscopic debridement, and microfracture and drilling to help stimulate cartilage growth.
This procedure, along with lifestyle changes that included eliminating all high-impact activities, bought me over 20 years of good mobility with manageable pain. Once I hit my fifties with an injury over 30 years old, my quality of life was once again compromised with limited motion and bad pain.
Dr. Ferkel then suggested viscosupplementation, an ankle injection procedure with lubricating fluid. It is also called hyaluronic acid injections and commonly used to treat knee osteoarthritis. It was not FDA approved for ankles (and insurance would not cover it), but I wanted to proceed if it meant a decrease in pain and an increase in mobility. It worked, and I did the injection every year for five years. After each injection, it felt like a little cushion in my ankle; there was a spring in my walk again. Acupuncture also greatly helped manage the pain when I could find the time to do it.
Although it was not a cure, my quality of life improved. When I traveled and needed to do a lot of walking, I would take Celebrex, (also know as a COX-2 inhibitor) a nonsteroidal anti-inflammatory drug (NSAID) that works by reducing hormones that cause inflammation and pain in the body.
There were no real fixes, just management options. Total ankle replacements (TAR) only last about eight to ten years, so that was not an option either. Fortunately for knees and hips total joint replacement surgery is an excellent option with longer-term beneficial results.
Looking at the end of my fifth decade, I was still not interested in ankle fusion, ankle arthrodesis, which can relieve pain but it also limits motion. I still had decent ankle motion and an ankle fusion would reduce existing mobility. My other fear was it could compromise other functioning joints that would eventually become taxed when the injured ankle joint was no longer mobile.
After extensive research there was promise for adult stem cell therapy that is an intervention strategy that introduces new adult stem cells into damaged tissue in order to treat disease or injury.
Stem cells are unprogrammed cells in the human body that have the ability to change or “differentiate” into other types of cells. Since they are obtained from the patient, the risk of rejection is almost non-existent. Knees have shown good results with stem cell therapy.
A 2014 study revealed that mesenchymal stem cell (MSCs) therapy on knees with osteoarthritis had the potential for cartilage regeneration. Today this procedure is considered a reliable alternative treatment for chronic knee OA.
Ankles are still the last frontier in this area. After 40 years since the initial injury, the biomechanical changes across my ankle joint surface had produced severe osteoarthritis. Daily walking became so painful I started planning my day around managing how much walking was needed to accomplish basic life duties.
I had dreams about running, and being free to move without pain. Friends no longer called to go hiking or power walking. It was difficult to maintain a healthy weight without being able to just simply walk. I was envious of friends who counted steps to lose weight, I planned my day around how few steps were needed to survive daily tasks.
Something had to be done, and it wasn’t going to be ankle fusion. That said, I spoke with many people who opted for ankle fusion and it changed their lives. Many even returned to athletic hobbies.
Stem cell therapy was my next move and Dr. Ferkel felt it could be a good option to help reduce pain and increase mobility.
It was an “experimental” procedure because it is not yet FDA approved. Based on research using stem cells from the iliac crest (hip bone), it had promise.
Dr. Ferkel told me,
My future was changed forever when I sprained my ankle in a college ballet class. This injury was 40 years ago yet a third degree sprain like mine was treated the same way as today: P-R-I-C-E (protect from further injury, restrict activity, apply ice, apply compression, and elevate the injured area).
Little did I know that the ligaments I injured had started physiological changes that would compromise my joint stability. The healing response that was initiated in an attempt to repair the damage actually increased my risk for degenerative changes that eventually led to osteoarthritis. It is the most common type of arthritis caused by the degradation of a joint’s cartilage. There are up to two million acute ankle sprains each year in just the USA alone.
Fifteen years after the initial ankle sprain I had severe pain and was forced to seek out medical attention in an attempt to walk normally again. Being in my mid-thirties and hearing that my only option was an ankle fusion, limiting motion for the rest of my life, was devastating news. My new mission was to find an ankle expert that was a pioneer.
NOTE reference photo of my left ankle X-ray 40 years after the injury, bone on bone, compared to a healthy normal ankle on the right side.
After five appointments with orthopedic surgeons in the Los Angeles area, I discovered Dr. Richard Ferkel at the Southern California Orthopedic Institute (SCOI). He became my lifetime ankle hero. He specializes in arthroscopic and reconstructive surgery of the ankle, as well as cartilage restoration, but it was his work with the U.S. Olympic teams, the NFL and NBA that really impressed me. If professional athletes entrusted their careers and joints to him, so would I.
Dr. Ferkel did a procedure to clean up the bone spurs, called arthroscopic debridement, and microfracture and drilling to help stimulate cartilage growth.
This procedure, along with lifestyle changes that included eliminating all high-impact activities, bought me over 20 years of good mobility with manageable pain. Once I hit my fifties with an injury over 30 years old, my quality of life was once again compromised with limited motion and bad pain.
Dr. Ferkel then suggested viscosupplementation, an ankle injection procedure with lubricating fluid. It is also called hyaluronic acid injections and commonly used to treat knee osteoarthritis. It was not FDA approved for ankles (and insurance would not cover it), but I wanted to proceed if it meant a decrease in pain and an increase in mobility. It worked, and I did the injection every year for five years. After each injection, it felt like a little cushion in my ankle; there was a spring in my walk again. Acupuncture also greatly helped manage the pain when I could find the time to do it.
Although it was not a cure, my quality of life improved. When I traveled and needed to do a lot of walking, I would take Celebrex, (also know as a COX-2 inhibitor) a nonsteroidal anti-inflammatory drug (NSAID) that works by reducing hormones that cause inflammation and pain in the body.
There were no real fixes, just management options. Total ankle replacements (TAR) only last about eight to ten years, so that was not an option either. Fortunately for knees and hips total joint replacement surgery is an excellent option with longer-term beneficial results.
Looking at the end of my fifth decade, I was still not interested in ankle fusion, ankle arthrodesis, which can relieve pain but it also limits motion. I still had decent ankle motion and an ankle fusion would reduce existing mobility. My other fear was it could compromise other functioning joints that would eventually become taxed when the injured ankle joint was no longer mobile.
After extensive research there was promise for adult stem cell therapy that is an intervention strategy that introduces new adult stem cells into damaged tissue in order to treat disease or injury.
Stem cells are unprogrammed cells in the human body that have the ability to change or “differentiate” into other types of cells. Since they are obtained from the patient, the risk of rejection is almost non-existent. Knees have shown good results with stem cell therapy.
A 2014 study revealed that mesenchymal stem cell (MSCs) therapy on knees with osteoarthritis had the potential for cartilage regeneration. Today this procedure is considered a reliable alternative treatment for chronic knee OA.
Ankles are still the last frontier in this area. After 40 years since the initial injury, the biomechanical changes across my ankle joint surface had produced severe osteoarthritis. Daily walking became so painful I started planning my day around managing how much walking was needed to accomplish basic life duties.
I had dreams about running, and being free to move without pain. Friends no longer called to go hiking or power walking. It was difficult to maintain a healthy weight without being able to just simply walk. I was envious of friends who counted steps to lose weight, I planned my day around how few steps were needed to survive daily tasks.
Something had to be done, and it wasn’t going to be ankle fusion. That said, I spoke with many people who opted for ankle fusion and it changed their lives. Many even returned to athletic hobbies.
Stem cell therapy was my next move and Dr. Ferkel felt it could be a good option to help reduce pain and increase mobility.
It was an “experimental” procedure because it is not yet FDA approved. Based on research using stem cells from the iliac crest (hip bone), it had promise.
Dr. Ferkel told me,
“The goal is to reduce pain and keep mobility.”He knew I had a fantasy that those stem cells would grow new cartilage, which it would not in my case of almost total bone on bone. For many who have a smaller injury, stem cells are now an excellent option, even on ankles. During the surgery they had to collect the stem cells from the hip joint and distract my ankle joint (separate it from my leg) for the injection of bone marrow aspirate. Concentrated bone marrow aspirate contains healing and growth factors, as well as healing cells called pluripotent cells. Bone marrow is the tissue that is found in the hollow spaces in the interior of our bones.
 A centrifugation machine called the Magellan® MAR0Max™ was used to concentrate the platelets and growth factors, as well as the pluripotent (or stem) cells, creating an injectable product that is delivered directly to the ankle. The processing time is about 12-17 minutes, and the entire surgery was less than an hour.
My personal ankle plan now is to wait for another ten years until I am a candidate for a total ankle replacement. I will continue to utilize hyaluronic acid injections, take Celebrex when needed and be open to new options until it is time for my total ankle replacement.
We are all different, and fortunately there are good options available for ankle osteoarthritis now.
My hope is that those with similar injuries catch it early so new treatments like stem cell therapy may stop the progression of osteoarthritis, and joint replacements become a thing of the past for everyone.
By Staness Jonekos
*************************************************************************************
References:
Wodicka R, Ferkel E, Ferkel R. Osteochondral Lesions of the Ankle. Foot Ankle Int. 2016 Sep;37(9):1023-34.
Ramponi L, Yasui Y, Murawski CD, Ferkel RD, DiGiovanni CW, Kerkhoffs GM, Calder JD, Takao M, Vannini F, Choi WJ, Lee JW, Stone J, Kennedy JG. Lesion Size Is a Predictor of Clinical Outcomes After Bone Marrow Stimulation for Osteochondral Lesions of the Talus: A Systematic Review. Am J Sports Med. 2016 Nov 16. pii: 0363546516668292.
Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, Kim JE, Shim H, Shin JS, Shin IS, Ra JC, Oh S, Yoon KS. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014 May;32(5):1254-66.
Mehrabani D, Mojtahed Jaberi F, Zakerinia M, Hadianfard MJ, Jalli R, Tanideh N, Zare S.
The Healing Effect of Bone Marrow-Derived Stem Cells in Knee Osteoarthritis: A Case Report. World J Plast Surg. 2016 May;5(2):168-74.
Burke J, Hunter M, Kolhe R, Isales C, Hamrick M, Fulzele S. Therapeutic potential of mesenchymal stem cell based therapy for osteoarthritis. Clin Transl Med. 2016 Dec;5(1):27.
A centrifugation machine called the Magellan® MAR0Max™ was used to concentrate the platelets and growth factors, as well as the pluripotent (or stem) cells, creating an injectable product that is delivered directly to the ankle. The processing time is about 12-17 minutes, and the entire surgery was less than an hour.
My personal ankle plan now is to wait for another ten years until I am a candidate for a total ankle replacement. I will continue to utilize hyaluronic acid injections, take Celebrex when needed and be open to new options until it is time for my total ankle replacement.
We are all different, and fortunately there are good options available for ankle osteoarthritis now.
My hope is that those with similar injuries catch it early so new treatments like stem cell therapy may stop the progression of osteoarthritis, and joint replacements become a thing of the past for everyone.
By Staness Jonekos
*************************************************************************************
References:
Wodicka R, Ferkel E, Ferkel R. Osteochondral Lesions of the Ankle. Foot Ankle Int. 2016 Sep;37(9):1023-34.
Ramponi L, Yasui Y, Murawski CD, Ferkel RD, DiGiovanni CW, Kerkhoffs GM, Calder JD, Takao M, Vannini F, Choi WJ, Lee JW, Stone J, Kennedy JG. Lesion Size Is a Predictor of Clinical Outcomes After Bone Marrow Stimulation for Osteochondral Lesions of the Talus: A Systematic Review. Am J Sports Med. 2016 Nov 16. pii: 0363546516668292.
Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, Kim JE, Shim H, Shin JS, Shin IS, Ra JC, Oh S, Yoon KS. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014 May;32(5):1254-66.
Mehrabani D, Mojtahed Jaberi F, Zakerinia M, Hadianfard MJ, Jalli R, Tanideh N, Zare S.
The Healing Effect of Bone Marrow-Derived Stem Cells in Knee Osteoarthritis: A Case Report. World J Plast Surg. 2016 May;5(2):168-74.
Burke J, Hunter M, Kolhe R, Isales C, Hamrick M, Fulzele S. Therapeutic potential of mesenchymal stem cell based therapy for osteoarthritis. Clin Transl Med. 2016 Dec;5(1):27. Do Menopause and Alcohol Mix?
 You’ve probably heard that moderate drinking is good for your heart. But you’ve probably also heard that it’s a danger for breast cancer and that it can trigger hot flashes. Here are the facts that can help you make decisions about drinking.
The most important thing is how much you drink. The benefits come with moderate—big emphasis on moderate—drinking. Starting with the Framingham Heart Study, big epidemiologic studies have shown that while moderate drinking has some benefits, drinking much more than that can be detrimental. More than two drinks per day and the negative effects begin to pile up, with increases in the rates of cancer, stroke, and more.
You’ve probably heard that moderate drinking is good for your heart. But you’ve probably also heard that it’s a danger for breast cancer and that it can trigger hot flashes. Here are the facts that can help you make decisions about drinking.
The most important thing is how much you drink. The benefits come with moderate—big emphasis on moderate—drinking. Starting with the Framingham Heart Study, big epidemiologic studies have shown that while moderate drinking has some benefits, drinking much more than that can be detrimental. More than two drinks per day and the negative effects begin to pile up, with increases in the rates of cancer, stroke, and more.
What’s One Drink?
This is how the National Institute on Alcohol Abuse and Alcoholism (NIAA) defines one standard drink:- 5 fluid ounces (one glass) of wine (about 12% alcohol). Don’t let your wine glass fool you—most hold much more than 5 ounces.
- 12 fluid ounces (usually one can or bottle) of regular beer (about 5% alcohol)
- 1.5 fluid ounces (one shot) of 80-proof distilled spirits
- Light: less than one drink per day
- Moderate: one to two drinks per day
- Heavy: more than two drinks per day
How Much Is Good?
- Light to moderate drinkers have a significantly lower risk of coronary heart disease than nondrinkers. For women, the heart benefits of moderate drinking become apparent at menopause when their heart disease risk normally goes up, and the heart benefits continue after that. Hormone therapy doesn’t affect that benefit.
- Women who drink moderately have a lower risk of type 2 diabetes.
- Those who drink moderate amounts of alcohol, especially wine, have a lower risk of dementia than those who don’t drink at all.
- Women who drink lightly or moderately have a lower risk of stroke than nondrinkers.
- At and after menopause (ages 50-62), women who drink moderately have stronger bones than nondrinkers.
- Midlife and older women who drink lightly or moderately have a lower risk of becoming obese than nondrinkers.
How Much Is Bad?
- Drinking may trigger hot flashes for some women, although that isn’t based in research. So determine whether it’s a personal trigger for you. (As for a general risk of experiencing hot flashes and night sweats, some studies find alcohol increases it, whereas others find the opposite.)
- Any amount of alcohol increases the risk of breast cancer. The increase in risk is there, but small, for women who drink one drink a day. Women who drink two to five drinks a day have about 1.5 times the risk of nondrinkers. (The increased risk doesn’t seem to have anything to do with alcohol’s effect on estrogen levels.)
- Drinking alcohol increases the risk of many other cancers. The risk rises with the amount of alcohol consumed. (And the risk rises higher if you smoke as well.)
- Alcohol has harmful interactions with many medications, even ones you may not think about, such as medicines for arthritis, indigestion or heartburn, high cholesterol, high blood pressure, and more. Check out which ones here.
- More than moderate drinking increases the risk of cardiovascular disease. Among heavy drinkers, women are more susceptible to alcohol-related heart disease than men.
- Women who drink heavily are prone to central obesity—the apple shape that is a big risk for cardiovascular disease.
- Heavy drinking can lead to osteoporosis that cannot be reversed. It’s also a risk for fractures.
- Binge drinking increases the risk of developing type 2 diabetes.
- Women at menopause are especially vulnerable to depression, and heavy drinking can just make that worse. Heavy drinking itself can lead to depression, and women who show signs of alcoholism are two to seven times more at risk of developing depression than men.
- Alcoholic women are more susceptible than men to key organ system damage, including heart muscle damage, nerve damage, cirrhosis, and possibly brain damage as well.
Take It Easy
If you drink alcohol, enjoy yourself, but make sure your drinking is light to moderate. For women, the NIAA puts its low-risk drinking limit at no more than seven drinks a week and no more than three drinks on any single day. Provided by: The North American Menopause SocietyCan Red Wine Reduce Your Risk for Breast Cancer?
Learn More:
Need to know more about alcohol and your health? Try the NIAA’s Rethinking Drinkingsite.downloads
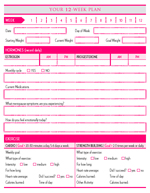
FREE essential planner downloads! Create your own personalized Menopause Makeover planner! Set goals and track results, document symptoms, journal your feelings, prepare your food plan and shopping lists. Click here (not image)